Engaging Adolescents and Young Adults to Get Tested
An STD Awareness Month blog highlighting some creative and innovative ways of providing STD services to young people across the US.

Sexually transmitted infections are at a 20-year high in the United States. STDs disproportionately affect adolescents and young adults aged 15-24, with this age group making up half of the new STD diagnosis’ each year. These rates only provide a snapshot of the true incidence because testing and screening are inconsistent and suboptimal due to barriers to access for young people, including, but not limited to, free/low cost confidential services, youth-friendly clinics and providers, and accurate sexual health education/information. Here are a few creative initiatives designed to tackle some of these barriers to access, including increasing access to testing and awareness of screening services.
Removing Barriers to Access
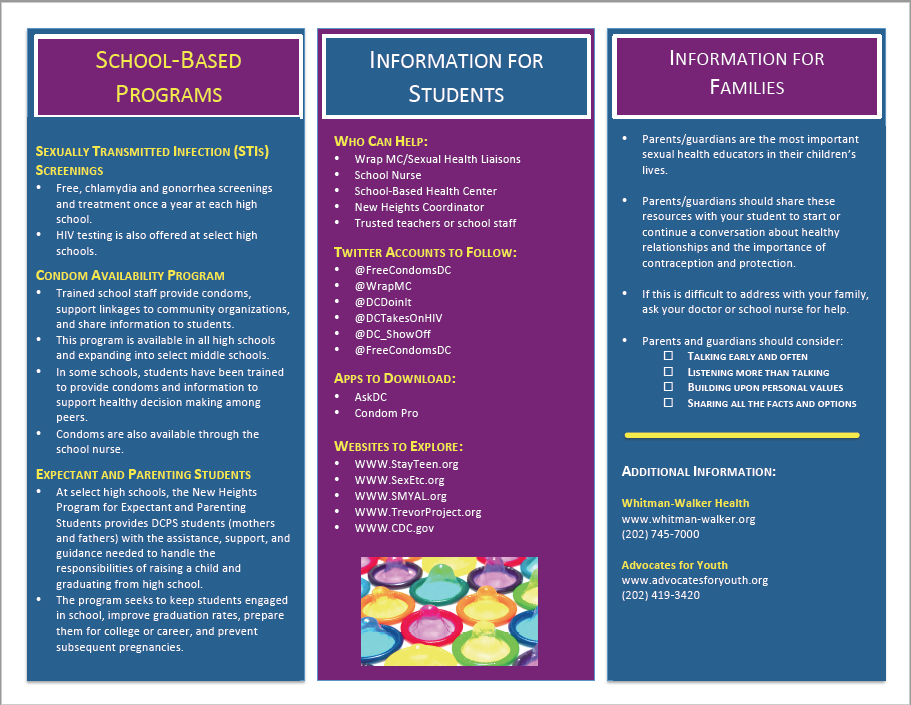
Public Schools – STD Screenings at High Schools
In many communities, a barrier to accessing STD testing is limited clinic hours. Many clinics operate Monday-Friday during hours which overlap with the school day, and most have limited hours on Saturdays. To address this barrier, several cities decided to bring testing to schools, meeting young people where they learn and spend most of their day. The Michigan health department developed a program to tackle the rising chlamydia rates among young people in the state by offering voluntary chlamydia screenings at four Detroit high schools. The program provided students with information on STD risk and addressed stigma around getting tested by normalizing testing and encouraging all students to participate in the program. If students tested positive for an STD, they were confidentially referred to a clinic for treatment and additional care as needed. The screening program was a huge success and resulted in a significant decrease in chlamydia cases in Detroit.
With rates of HIV, chlamydia, and gonorrhea in persons aged 13-24 far above the national average, the District of Columbia Public School system offers a similar annual voluntary screening of chlamydia and gonorrhea at most high schools. Before screening occurs, materials are sent home to help foster conversation between parents and students around sexual health. However, students do not require parental permission to participate in these screenings, which provides students with the ability to access critical sexual health services in a confidential way.
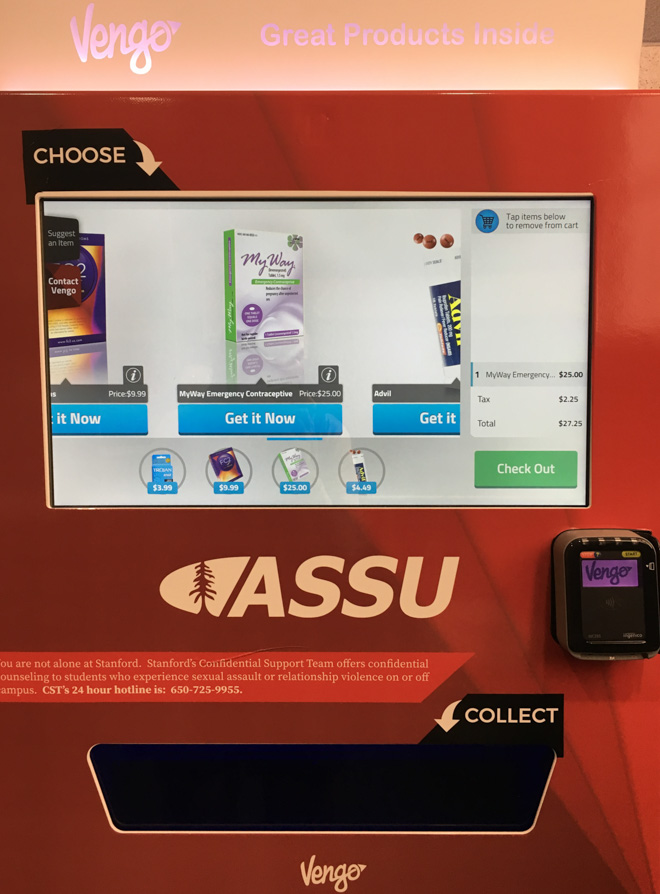
Opportunities on College Campuses – Access to Sexual Health Products
Several colleges across the nation are adding sexual health vending machines to their campuses. Currently, many of these vending machines include condoms, FC2 internal condoms, emergency contraceptives, pregnancy tests, and personal lubricants. Having these vending machines throughout college campuses makes it easy for students to quickly access important sexual health care products without having to travel far, or experience potentially awkward encounters with pharmacists or drug store employees. Additionally, when students buy from these machines, only the company name shows up on any bank statement, keeping the product purchase confidential.
Emerging evidence from a cross-sectional survey** at George Mason University in Fairfax, Virginia suggests that more college students might get tested if they could self-collect. The survey assessed students’ behaviors, attitudes, and intentions in regard to STD/HIV self-testing kits, and found that students were interested in self-testing services, and that they would be more likely to utilize self-test kits in the privacy of their own home instead of seeking traditional screening services if given the option. Students also reported that their concerns with self-testing kits were cost, accuracy, confidentiality, and clear “how to” instructions.
Addressing Stigma: Sex-Positive Approaches
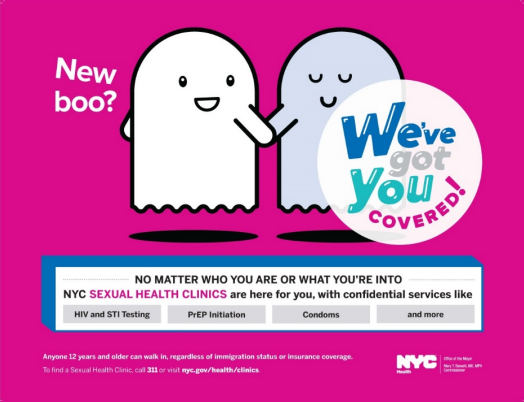
NYC Department of Health and Mental Hygiene – “We’ve Got You Covered” Campaign
In early 2017, the New York City Department of Health rebranded their STD services to become more inclusive of all sexual health needs. A component of the rebranding initiative was a media campaign—We’ve Got You Covered—focused on sexual health and sex-positive messaging. Sex-positive messaging reduces shame, stigma, and secrecy around sexual health heath, and does not make moral judgments about sexual orientation or behaviors. Campaign ads had simple designs with an emojicon style, speaking to the way young people consume information, and were posted throughout the city in train stations, bus stops, and store fronts. The ads provided important information about STD/HIV prevention, ages that could be served, testing and counseling services, and where to learn more in a simple and accessible way.

DC Department of Health, HIV/AIDS, Hepatitis, STD and TB Administration – “Sex Is…” Campaign
In 2017, DC Health launched their “Sex Is…” campaign which focuses on honest judgement-free conversation about sex and sexual health in young people. “Sex Is…” participates in events throughout DC promoting awareness of the campaign as well as educating the community on engaging in healthy positive conversations about sex with young people. “Sex Is…” also has a Youth Advisory Board comprised of DC residents aged 12-24, who are trained on how to have sexual health conversations with peers and adults, conduct community outreach, and develop campaign designs. The “Sex Is…” website also provides an easy to access and searchable list of locations which can meet a variety of health needs.

Concluding Thoughts & Ideas for Increasing Accessibility
Each of the initiatives highlighted above provides insight into what is being done in just a few areas of the country to ensure adolescents and young adults are able to lead happy, healthy lives. There are always opportunities to continue to improve and fill sexual health access gaps for young people. For example, an opportunity to increase youth testing rates is to make it more accessible by including low-cost STD/HIV self-testing kits within the sexual health vending machines on college campuses. Placing the low-cost self-testing kits in the vending machines helps address travel, time, and financial barriers that students often face in accessing the same services in a clinic or other health care setting.
Although all of the initiatives outlined here have a healthcare consumer focus, providers play an important role in the prevention conversation. Additional efforts should be taken to address the barriers providers face that prevent them from providing the best care possible. Some areas to consider are later clinic hours, more inclusive, youth-friendly screening language, and increasing the time spent with patients. In order to reverse the STD epidemic in America, we must continue to look for innovative solutions that address the barriers preventing young people from accessing the sexual health services they need and deserve.
**Peer reviewed journal article pending